Guest blog by
Julie McGee
As a physical therapist, this is my motto. This also applies to runners. In running, the idea is to move quickly to propel the body forward while being upright. If you are running, and you core is weak, while your legs are strong you are going to run into some issues. You are going to hurt yourself.
Think of a pogo stick, that toy from our childhood. A pogo stick is basically a spring attached to a post that is surrounded by a stable base with handles and footrests. If the base is made of a strong, stable material such as steel, or aluminum, the user can propel themselves upwards, and if skillful enough, hop along. If the base is made of a less stable material such as cardboard, it is going to buckle and fold as the user tries to use it to hop and propel themselves forward.
Now apply the concept of a pogo stick, with a strong spring and post to your body. Even if your legs are strong, if your base is weak, when you try to propel yourself forward, your base (aka, your core) is going to buckle. As a result your body will make a lot of aberrant movements that over time will wear down on your body and result in injury.
There is evidence that core strength may help to prevent injuries in certain athlete groups (here). There is also research to suggest that a good core strength and stability exercise program can help to prevent lower extremity injury in a more general population (here). Specific to those suffering from patellafemoral pain syndrome, is some evidence that improved core strength may help with knee pain (here).
Before I get too carried away with exercise, let me speak a little about core strength, core stability, and the difference between the two. Core strength is the strength of the muscles in your trunk and hips. Core stability is the ability of those muscles to work effectively in stabilizing the trunk for one to perform functional movement (think lifting, running, and day to day activities).
Endurance athletes doing longer workouts, may have difficulty fitting core exercises in to their routine. If you only have 45 minutes, or an hour to workout on a weekday, you may choose to spend that time doing the endurance workout of your choice (for me, it’s typically running, biking, or swimming). However, spending a few of those minutes on your core may pay dividends over the course of time as you may experience fewer injuries, and be able to run a little faster.
Here are a few favorites:
- Quadraped progression
- Front and side plank
- Front and side plank with a leg lifted
As a challenge, planks can also be done with an exercise ball:
Since there is a rotational component to running, exercises that involve rotation, and work the obliques can also be effective:
Supine rotation: Lie on your back, with your arms out to the side so that you look like the letter, “T.” Lift your legs so that your hips and knees are bent. While keeping your shoulder blades on the ground, let your legs fall over to one side. Remember! Keep your shoulder blades on the ground! Otherwise you are just rolling around. Once you get to your limit, bring your legs back to he middle, and repeat on the other side.
Plank rotations with the exercise ball: Start off on a plank position where the exercise ball is under your feet. Lift one leg up and behind you. Then bring that leg down, and across your midline – almost as though you were going to tap the ground next to the other side of the ball. Repeat, as many times as you can tolerate. Then switch sides.
There are many more exercises out there. Classes such as yoga and pilates can also help to improve core strength. So look around you, and maybe grab an exercise ball.
About
Julie McGee, PT, DPT, CEAS
Julie McGee is a physical therapist with over 10 years of experience. During that time she has worked in acute rehab, worker’s comp, outpatient orthopedics, and home health. Through her work, Julie has found that she is passionate about writing and educating others whether they are patients or clinicians.
Julie received her B.S in Exercise Science in 2003. She then went on to receive her MSPT and DPT from the University of California, San Francisco/ San Francisco State University Graduate Program in Physical Therapy in 2007 and 2008 respectively.
Julie has had her writing published in Medium, NewGradPT.com, and CovalentCareers.com. She also writes for, and manages runningfrominjury.com, a blog that focuses on running related injuries and their prevention.
When she is not writing or treating patients, Julie can be found running, cycling, swimming, doing yoga, and reading a good book.
--
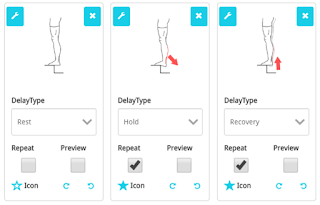
Julie has recommended some of her favorite core exercises which we have added into a home exercise program on the PT-Helper CONNECT platform and presented on the PT-Helper mobile app. These sample exercises can be quickly downloaded into the PT-Helper mobile app using
HEP code: 5FB98480
You can also find these exercises in the Fitness - Core category in the PT-Helper mobile app to add to your Favorites which allows you to customize each exercise’s repetitions, sets, and hold time.
Reminder: Please consult your physician before engaging in any physical activity and stop if you experience pain or discomfort.
Start your
Free 30-day Trial of the PT-Helper CONNECT tool for physical therapists and other therapy providers, so you too may create and prescribe Home Exercise Programs like the one shown above.
Click here to view
Fitness - Core exercises currently available within the PT-Helper Exercise Library.